Dialysis Nutrition and Weight Management

For people with chronic kidney disease (CKD) or end stage renal disease (ESRD), extra weight also increases the risk of type 2 diabetes and high blood pressure. Yearly kidney screening tests are suggested for everyone that is overweight, particularly those with diabetes or high blood pressure.
Making a few changes to your diet could prevent or lower your risk factors. And in some cases, it may even be the key to slowing down or stopping chronic diseases like diabetes, high blood pressure and cardiovascular disease. If you are overweight, it’s important to manage what you eat along with help from your renal dietitian.
Why all the weigh-ins?
Your weight affects how much fluid to remove during dialysis. Your doctor and nurses will determine your dialysis estimated dry weight without extra fluid.
If your kidneys start to put out less fluid than you take in, fluid will build up in your body, which is not good. Dialysis can remove most of this extra fluid, but not all.
Large weight changes can cause blood pressure changes, headaches, leg cramps, breathing problems and other issues. To prevent these problems, you may need to drink or eat less than 4 to 5 cups of fluid a day.
Some people lose weight before starting treatment. However, you will start to feel better and regain your appetite. Just know that you should only expect to gain perhaps 1 to 2 pounds a week of actual body weight, not fluid weight.
Controlling how much you drink isn’t always easy, but you can do it. Just be mindful and follow the plan that your dietitian has created for you. Managing your fluid intake will help you feel better on dialysis and keep you in better health.

Excess fluid in your body shows up on the scale. Limiting fluids will help you feel better and stay healthier.
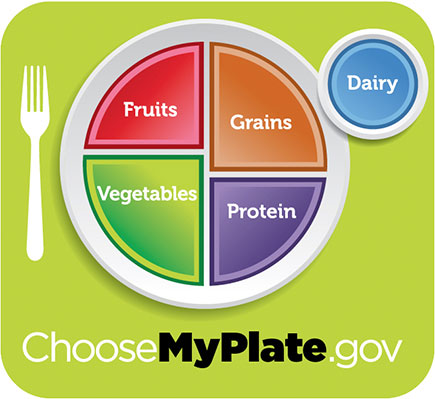
Proper portions for weight control
Nutrition for people on dialysis
Along with receiving your full dialysis treatment on schedule, managing what you eat and drink is one of the biggest factors in your long-term health and your success on dialysis. Your renal (kidney) dietitian will work with you to develop a CKD diet plan that’s customized to your exact nutritional needs—and incorporates all of your favorite flavors.
Looking for cooking inspiration? Find delicious, kidney-friendly recipes in our downloadable cookbook collection.
